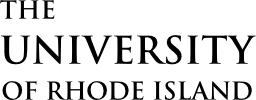
Tick Finder Tool
Find a tick? Or just curious about tick activity in your region? Maybe you want to discover tick encounter risk across the country before your next trip? Pick a date and pick a region, then use our tool to get started.
Tick Activity
Select a region to begin searching for ticks, and adjust the time of year to see how tick activity changes.
Results will appear here, sorted from most to least active.
Northeast Central
January
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 1Blacklegged (Deer) TickLarvaInactive
1Blacklegged (Deer) TickLarvaInactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive 5Blacklegged (Deer) TickNymphInactive
5Blacklegged (Deer) TickNymphInactive 2Lone Star TickAdult FemaleInactive
2Lone Star TickAdult FemaleInactive Lone Star TickLarvaInactive
Lone Star TickLarvaInactive 2Lone Star TickNymphInactive
2Lone Star TickNymphInactive
February
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 1Blacklegged (Deer) TickLarvaInactive
1Blacklegged (Deer) TickLarvaInactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive 5Blacklegged (Deer) TickNymphInactive
5Blacklegged (Deer) TickNymphInactive 2Lone Star TickAdult FemaleInactive
2Lone Star TickAdult FemaleInactive Lone Star TickLarvaInactive
Lone Star TickLarvaInactive 2Lone Star TickNymphInactive
2Lone Star TickNymphInactive
March
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity
April
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity
May
 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity
June
 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
July
 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity Gulf Coast TickAdult MaleActivity
Gulf Coast TickAdult MaleActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity
August
 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity American Dog TickLarvaActivity
American Dog TickLarvaActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Inactive
5Blacklegged (Deer) TickAdult Female (Fully Fed)Inactive
September
 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity American Dog TickLarvaActivity
American Dog TickLarvaActivity 5Blacklegged (Deer) TickAdult FemaleInactive
5Blacklegged (Deer) TickAdult FemaleInactive 2Lone Star TickNymphInactive
2Lone Star TickNymphInactive 5Blacklegged (Deer) TickAdult Female (Partially Fed)Inactive
5Blacklegged (Deer) TickAdult Female (Partially Fed)Inactive 2Lone Star TickAdult MaleInactive
2Lone Star TickAdult MaleInactive 5Blacklegged (Deer) TickAdult Female (Fully Fed)Inactive
5Blacklegged (Deer) TickAdult Female (Fully Fed)Inactive Brown Dog TickAdult FemaleInactive
Brown Dog TickAdult FemaleInactive Brown Dog TickAdult MaleInactive
Brown Dog TickAdult MaleInactive
October
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive 2Lone Star TickAdult FemaleInactive
2Lone Star TickAdult FemaleInactive Lone Star TickLarvaInactive
Lone Star TickLarvaInactive 2Lone Star TickNymphInactive
2Lone Star TickNymphInactive
November
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive Brown Dog TickAdult Female (Fully Fed)Inactive
Brown Dog TickAdult Female (Fully Fed)Inactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive
December
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive Brown Dog TickAdult Female (Fully Fed)Inactive
Brown Dog TickAdult Female (Fully Fed)Inactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive 1Blacklegged (Deer) TickLarvaInactive
1Blacklegged (Deer) TickLarvaInactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive
Southeast Central
January
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult FemaleInactive
2Lone Star TickAdult FemaleInactive American Dog TickLarvaInactive
American Dog TickLarvaInactive
February
 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity
March
 American Dog TickLarvaActivity
American Dog TickLarvaActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 2Gulf Coast TickNymphActivity
2Gulf Coast TickNymphActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
April
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity American Dog TickLarvaActivity
American Dog TickLarvaActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
May
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity American Dog TickNymphActivity
American Dog TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity
June
 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2Lone Star TickAdult Female (Partially Fed)Activity
2Lone Star TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult Female (Fully Fed)Activity
2Lone Star TickAdult Female (Fully Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity American Dog TickNymphActivity
American Dog TickNymphActivity
July
 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2Lone Star TickAdult Female (Partially Fed)Activity
2Lone Star TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult Female (Fully Fed)Activity
2Lone Star TickAdult Female (Fully Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
August
 Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity American Dog TickLarvaActivity
American Dog TickLarvaActivity
September
 Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity American Dog TickLarvaActivity
American Dog TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity
October
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity
November
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity
December
 Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2Lone Star TickAdult MaleInactive
2Lone Star TickAdult MaleInactive
Mid Atlantic
January
 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult FemaleInactive
2Lone Star TickAdult FemaleInactive American Dog TickLarvaInactive
American Dog TickLarvaInactive Lone Star TickLarvaInactive
Lone Star TickLarvaInactive American Dog TickNymphInactive
American Dog TickNymphInactive 2Lone Star TickNymphInactive
2Lone Star TickNymphInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive
February
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2Lone Star TickAdult MaleInactive
2Lone Star TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive Brown Dog TickAdult FemaleInactive
Brown Dog TickAdult FemaleInactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive Brown Dog TickAdult MaleInactive
Brown Dog TickAdult MaleInactive
March
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 2Gulf Coast TickNymphActivity
2Gulf Coast TickNymphActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity
April
 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity American Dog TickNymphActivity
American Dog TickNymphActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
May
 American Dog TickLarvaActivity
American Dog TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity American Dog TickNymphActivity
American Dog TickNymphActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity
June
 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity American Dog TickLarvaActivity
American Dog TickLarvaActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity
July
 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity
August
 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity
September
 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity American Dog TickLarvaActivity
American Dog TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2Lone Star TickAdult MaleInactive
2Lone Star TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive Brown Dog TickAdult FemaleInactive
Brown Dog TickAdult FemaleInactive
October
 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity
November
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity Brown Dog TickAdult MaleInactive
Brown Dog TickAdult MaleInactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive Brown Dog TickAdult Female (Partially Fed)Inactive
Brown Dog TickAdult Female (Partially Fed)Inactive
December
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2Lone Star TickAdult MaleInactive
2Lone Star TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive Brown Dog TickAdult FemaleInactive
Brown Dog TickAdult FemaleInactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive Brown Dog TickAdult MaleInactive
Brown Dog TickAdult MaleInactive
Mountain
January
 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2Gulf Coast TickNymphInactive
2Gulf Coast TickNymphInactive 2Gulf Coast TickAdult FemaleInactive
2Gulf Coast TickAdult FemaleInactive 2Gulf Coast TickAdult MaleInactive
2Gulf Coast TickAdult MaleInactive 4Rocky Mountain Wood TickAdult FemaleInactive
4Rocky Mountain Wood TickAdult FemaleInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 4Rocky Mountain Wood TickAdult MaleInactive
4Rocky Mountain Wood TickAdult MaleInactive
February
 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive 4Rocky Mountain Wood TickNymphInactive
4Rocky Mountain Wood TickNymphInactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive
March
 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2Gulf Coast TickNymphActivity
2Gulf Coast TickNymphActivity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive 4Rocky Mountain Wood TickNymphInactive
4Rocky Mountain Wood TickNymphInactive
April
 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity 2Gulf Coast TickNymphActivity
2Gulf Coast TickNymphActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive 4Rocky Mountain Wood TickNymphInactive
4Rocky Mountain Wood TickNymphInactive
May
 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
June
 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
July
 Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity
August
 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive
September
 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2Gulf Coast TickNymphInactive
2Gulf Coast TickNymphInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive
October
 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2Gulf Coast TickNymphInactive
2Gulf Coast TickNymphInactive 2Gulf Coast TickAdult FemaleInactive
2Gulf Coast TickAdult FemaleInactive 2Gulf Coast TickAdult MaleInactive
2Gulf Coast TickAdult MaleInactive 4Rocky Mountain Wood TickAdult FemaleInactive
4Rocky Mountain Wood TickAdult FemaleInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive
November
 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 4Rocky Mountain Wood TickAdult FemaleInactive
4Rocky Mountain Wood TickAdult FemaleInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 4Rocky Mountain Wood TickAdult MaleInactive
4Rocky Mountain Wood TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive 4Rocky Mountain Wood TickNymphInactive
4Rocky Mountain Wood TickNymphInactive
December
 Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 1Brown Dog TickAdult FemaleActivity
1Brown Dog TickAdult FemaleActivity 1Brown Dog TickAdult MaleActivity
1Brown Dog TickAdult MaleActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 4Rocky Mountain Wood TickAdult MaleInactive
4Rocky Mountain Wood TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive 4Rocky Mountain Wood TickNymphInactive
4Rocky Mountain Wood TickNymphInactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive 4Rocky Mountain Wood TickLarvaInactive
4Rocky Mountain Wood TickLarvaInactive
New England
January
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive Brown Dog TickAdult MaleInactive
Brown Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive Brown Dog TickAdult Female (Partially Fed)Inactive
Brown Dog TickAdult Female (Partially Fed)Inactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive Brown Dog TickAdult Female (Fully Fed)Inactive
Brown Dog TickAdult Female (Fully Fed)Inactive
February
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Brown Dog TickAdult Female (Fully Fed)Inactive
Brown Dog TickAdult Female (Fully Fed)Inactive 1Blacklegged (Deer) TickLarvaInactive
1Blacklegged (Deer) TickLarvaInactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive 6Blacklegged (Deer) TickNymphInactive
6Blacklegged (Deer) TickNymphInactive 2Lone Star TickAdult FemaleInactive
2Lone Star TickAdult FemaleInactive Lone Star TickLarvaInactive
Lone Star TickLarvaInactive
March
 American Dog TickLarvaActivity
American Dog TickLarvaActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity
April
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity American Dog TickLarvaActivity
American Dog TickLarvaActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2Lone Star TickAdult Female (Partially Fed)Activity
2Lone Star TickAdult Female (Partially Fed)Activity
May
 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity
June
 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2Lone Star TickAdult Female (Partially Fed)Activity
2Lone Star TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult Female (Fully Fed)Activity
2Lone Star TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity
July
 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2Lone Star TickAdult Female (Partially Fed)Activity
2Lone Star TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult Female (Fully Fed)Activity
2Lone Star TickAdult Female (Fully Fed)Activity American Dog TickNymphActivity
American Dog TickNymphActivity
August
 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity American Dog TickLarvaActivity
American Dog TickLarvaActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 6Blacklegged (Deer) TickAdult FemaleInactive
6Blacklegged (Deer) TickAdult FemaleInactive 6Blacklegged (Deer) TickAdult Female (Partially Fed)Inactive
6Blacklegged (Deer) TickAdult Female (Partially Fed)Inactive
September
 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity American Dog TickLarvaActivity
American Dog TickLarvaActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive Brown Dog TickAdult MaleInactive
Brown Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive Brown Dog TickAdult Female (Partially Fed)Inactive
Brown Dog TickAdult Female (Partially Fed)Inactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive Brown Dog TickAdult Female (Fully Fed)Inactive
Brown Dog TickAdult Female (Fully Fed)Inactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive
October
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive Brown Dog TickAdult MaleInactive
Brown Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive
November
 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 1Blacklegged (Deer) TickLarvaActivity
1Blacklegged (Deer) TickLarvaActivity 6Blacklegged (Deer) TickNymphActivity
6Blacklegged (Deer) TickNymphActivity 2Lone Star TickAdult Female (Partially Fed)Inactive
2Lone Star TickAdult Female (Partially Fed)Inactive American Dog TickLarvaInactive
American Dog TickLarvaInactive 2Lone Star TickAdult Female (Fully Fed)Inactive
2Lone Star TickAdult Female (Fully Fed)Inactive American Dog TickNymphInactive
American Dog TickNymphInactive
December
 6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
6Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 6Blacklegged (Deer) TickAdult FemaleActivity
6Blacklegged (Deer) TickAdult FemaleActivity 6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
6Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult Female (Partially Fed)Inactive
2Lone Star TickAdult Female (Partially Fed)Inactive American Dog TickLarvaInactive
American Dog TickLarvaInactive 2Lone Star TickAdult Female (Fully Fed)Inactive
2Lone Star TickAdult Female (Fully Fed)Inactive American Dog TickNymphInactive
American Dog TickNymphInactive Brown Dog TickAdult FemaleInactive
Brown Dog TickAdult FemaleInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive
Pacific
January
 4Western-Blacklegged TickAdult FemaleActivity
4Western-Blacklegged TickAdult FemaleActivity 4Western-Blacklegged TickAdult MaleActivity
4Western-Blacklegged TickAdult MaleActivity 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive
February
 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity 4Western-Blacklegged TickAdult FemaleActivity
4Western-Blacklegged TickAdult FemaleActivity 4Western-Blacklegged TickAdult MaleActivity
4Western-Blacklegged TickAdult MaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity
March
 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity 4Western-Blacklegged TickNymphActivity
4Western-Blacklegged TickNymphActivity Western-Blacklegged TickLarvaActivity
Western-Blacklegged TickLarvaActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity
April
 4Western-Blacklegged TickNymphActivity
4Western-Blacklegged TickNymphActivity Western-Blacklegged TickLarvaActivity
Western-Blacklegged TickLarvaActivity 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
May
 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 4Western-Blacklegged TickNymphActivity
4Western-Blacklegged TickNymphActivity Western-Blacklegged TickLarvaActivity
Western-Blacklegged TickLarvaActivity
June
 4Western-Blacklegged TickNymphActivity
4Western-Blacklegged TickNymphActivity Western-Blacklegged TickLarvaActivity
Western-Blacklegged TickLarvaActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity
July
 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 4Western-Blacklegged TickNymphActivity
4Western-Blacklegged TickNymphActivity Western-Blacklegged TickLarvaActivity
Western-Blacklegged TickLarvaActivity
August
 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 4Western-Blacklegged TickNymphActivity
4Western-Blacklegged TickNymphActivity Western-Blacklegged TickLarvaActivity
Western-Blacklegged TickLarvaActivity 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity
September
 Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 4Rocky Mountain Wood TickAdult FemaleActivity
4Rocky Mountain Wood TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 4Rocky Mountain Wood TickAdult MaleActivity
4Rocky Mountain Wood TickAdult MaleActivity
October
 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 4Western-Blacklegged TickAdult FemaleActivity
4Western-Blacklegged TickAdult FemaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 4Western-Blacklegged TickAdult MaleActivity
4Western-Blacklegged TickAdult MaleActivity 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive
November
 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 4Western-Blacklegged TickAdult FemaleActivity
4Western-Blacklegged TickAdult FemaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 4Western-Blacklegged TickAdult MaleActivity
4Western-Blacklegged TickAdult MaleActivity 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive
December
 4Western-Blacklegged TickAdult FemaleActivity
4Western-Blacklegged TickAdult FemaleActivity 4Western-Blacklegged TickAdult MaleActivity
4Western-Blacklegged TickAdult MaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 4Pacific Coast TickAdult FemaleActivity
4Pacific Coast TickAdult FemaleActivity 4Pacific Coast TickAdult MaleActivity
4Pacific Coast TickAdult MaleActivity 4Rocky Mountain Wood TickAdult MaleInactive
4Rocky Mountain Wood TickAdult MaleInactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive
South Atlantic
January
 Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2Lone Star TickAdult Female (Partially Fed)Inactive
2Lone Star TickAdult Female (Partially Fed)Inactive
February
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
March
 American Dog TickLarvaActivity
American Dog TickLarvaActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 2Gulf Coast TickNymphActivity
2Gulf Coast TickNymphActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
April
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity American Dog TickLarvaActivity
American Dog TickLarvaActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity
May
 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity American Dog TickNymphActivity
American Dog TickNymphActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity
June
 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult Female (Partially Fed)Activity
2Lone Star TickAdult Female (Partially Fed)Activity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2Lone Star TickAdult Female (Fully Fed)Activity
2Lone Star TickAdult Female (Fully Fed)Activity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity
July
 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2Lone Star TickAdult Female (Partially Fed)Activity
2Lone Star TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult Female (Fully Fed)Activity
2Lone Star TickAdult Female (Fully Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
August
 Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity
September
 Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity
October
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity
November
 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity
December
 Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickLarvaInactive
Blacklegged (Deer) TickLarvaInactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive
Northwest Central
January
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Brown Dog TickAdult Female (Fully Fed)Inactive
Brown Dog TickAdult Female (Fully Fed)Inactive Blacklegged (Deer) TickLarvaInactive
Blacklegged (Deer) TickLarvaInactive 2Gulf Coast TickNymphInactive
2Gulf Coast TickNymphInactive 5Blacklegged (Deer) TickNymphInactive
5Blacklegged (Deer) TickNymphInactive 2Gulf Coast TickAdult FemaleInactive
2Gulf Coast TickAdult FemaleInactive 2Gulf Coast TickAdult MaleInactive
2Gulf Coast TickAdult MaleInactive
February
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 2Lone Star TickNymphInactive
2Lone Star TickNymphInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2Lone Star TickAdult MaleInactive
2Lone Star TickAdult MaleInactive 2American Dog TickAdult FemaleInactive
2American Dog TickAdult FemaleInactive Brown Dog TickAdult FemaleInactive
Brown Dog TickAdult FemaleInactive 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive
March
 2Gulf Coast TickNymphActivity
2Gulf Coast TickNymphActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity
April
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity
May
 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
June
 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity
July
 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity
August
 Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity
September
 Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity Brown Dog TickAdult Female (Fully Fed)Inactive
Brown Dog TickAdult Female (Fully Fed)Inactive 2Gulf Coast TickNymphInactive
2Gulf Coast TickNymphInactive 5Blacklegged (Deer) TickNymphInactive
5Blacklegged (Deer) TickNymphInactive Blacklegged (Deer) TickAdult MaleInactive
Blacklegged (Deer) TickAdult MaleInactive 5Blacklegged (Deer) TickAdult FemaleInactive
5Blacklegged (Deer) TickAdult FemaleInactive 2Lone Star TickAdult FemaleInactive
2Lone Star TickAdult FemaleInactive
October
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2Lone Star TickNymphInactive
2Lone Star TickNymphInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2Lone Star TickAdult MaleInactive
2Lone Star TickAdult MaleInactive
November
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive Brown Dog TickAdult MaleInactive
Brown Dog TickAdult MaleInactive 2American Dog TickAdult Female (Fully Fed)Inactive
2American Dog TickAdult Female (Fully Fed)Inactive
December
 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 2Gulf Coast TickAdult MaleInactive
2Gulf Coast TickAdult MaleInactive 2Lone Star TickAdult FemaleInactive
2Lone Star TickAdult FemaleInactive Lone Star TickLarvaInactive
Lone Star TickLarvaInactive 2Lone Star TickNymphInactive
2Lone Star TickNymphInactive 2American Dog TickAdult MaleInactive
2American Dog TickAdult MaleInactive 2Lone Star TickAdult MaleInactive
2Lone Star TickAdult MaleInactive
Southwest Central
January
 Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2American Dog TickAdult Female (Partially Fed)Inactive
2American Dog TickAdult Female (Partially Fed)Inactive 2Lone Star TickAdult Female (Fully Fed)Inactive
2Lone Star TickAdult Female (Fully Fed)Inactive
February
 Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity
March
 Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity American Dog TickLarvaActivity
American Dog TickLarvaActivity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity 2Gulf Coast TickNymphActivity
2Gulf Coast TickNymphActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity
April
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity American Dog TickLarvaActivity
American Dog TickLarvaActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
May
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity American Dog TickLarvaActivity
American Dog TickLarvaActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity
June
 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2Lone Star TickAdult MaleActivity
2Lone Star TickAdult MaleActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2Lone Star TickAdult Female (Partially Fed)Activity
2Lone Star TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult Female (Fully Fed)Activity
2Lone Star TickAdult Female (Fully Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity
July
 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2Lone Star TickAdult Female (Fully Fed)Activity
2Lone Star TickAdult Female (Fully Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity 2Lone Star TickAdult FemaleActivity
2Lone Star TickAdult FemaleActivity
August
 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Lone Star TickNymphActivity
2Lone Star TickNymphActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity 2American Dog TickAdult Female (Fully Fed)Activity
2American Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity
September
 Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity 2Gulf Coast TickAdult FemaleActivity
2Gulf Coast TickAdult FemaleActivity 2Gulf Coast TickAdult MaleActivity
2Gulf Coast TickAdult MaleActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity Lone Star TickLarvaActivity
Lone Star TickLarvaActivity 2American Dog TickAdult MaleActivity
2American Dog TickAdult MaleActivity 2American Dog TickAdult FemaleActivity
2American Dog TickAdult FemaleActivity 2American Dog TickAdult Female (Partially Fed)Activity
2American Dog TickAdult Female (Partially Fed)Activity
October
 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Blacklegged (Deer) TickLarvaActivity
Blacklegged (Deer) TickLarvaActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity
November
 Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickNymphActivity
5Blacklegged (Deer) TickNymphActivity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Gulf Coast TickLarvaActivity
Gulf Coast TickLarvaActivity
December
 Brown Dog TickAdult MaleActivity
Brown Dog TickAdult MaleActivity Brown Dog TickAdult Female (Partially Fed)Activity
Brown Dog TickAdult Female (Partially Fed)Activity Brown Dog TickAdult Female (Fully Fed)Activity
Brown Dog TickAdult Female (Fully Fed)Activity Blacklegged (Deer) TickAdult MaleActivity
Blacklegged (Deer) TickAdult MaleActivity 5Blacklegged (Deer) TickAdult FemaleActivity
5Blacklegged (Deer) TickAdult FemaleActivity 5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity
5Blacklegged (Deer) TickAdult Female (Partially Fed)Activity 5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity
5Blacklegged (Deer) TickAdult Female (Fully Fed)Activity Brown Dog TickAdult FemaleActivity
Brown Dog TickAdult FemaleActivity Blacklegged (Deer) TickLarvaInactive
Blacklegged (Deer) TickLarvaInactive 2Gulf Coast TickNymphInactive
2Gulf Coast TickNymphInactive
Jan
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
Additional Resources

Submit your tick
Help us keep track of tick activity across North America by submitting your tick to TickSpotters, our crowd-sourced tick survey. We’ll identify it for you and provide a risk assessment, prevention tips, and other resources to help you prepare for your next tick encounter.
Learn More