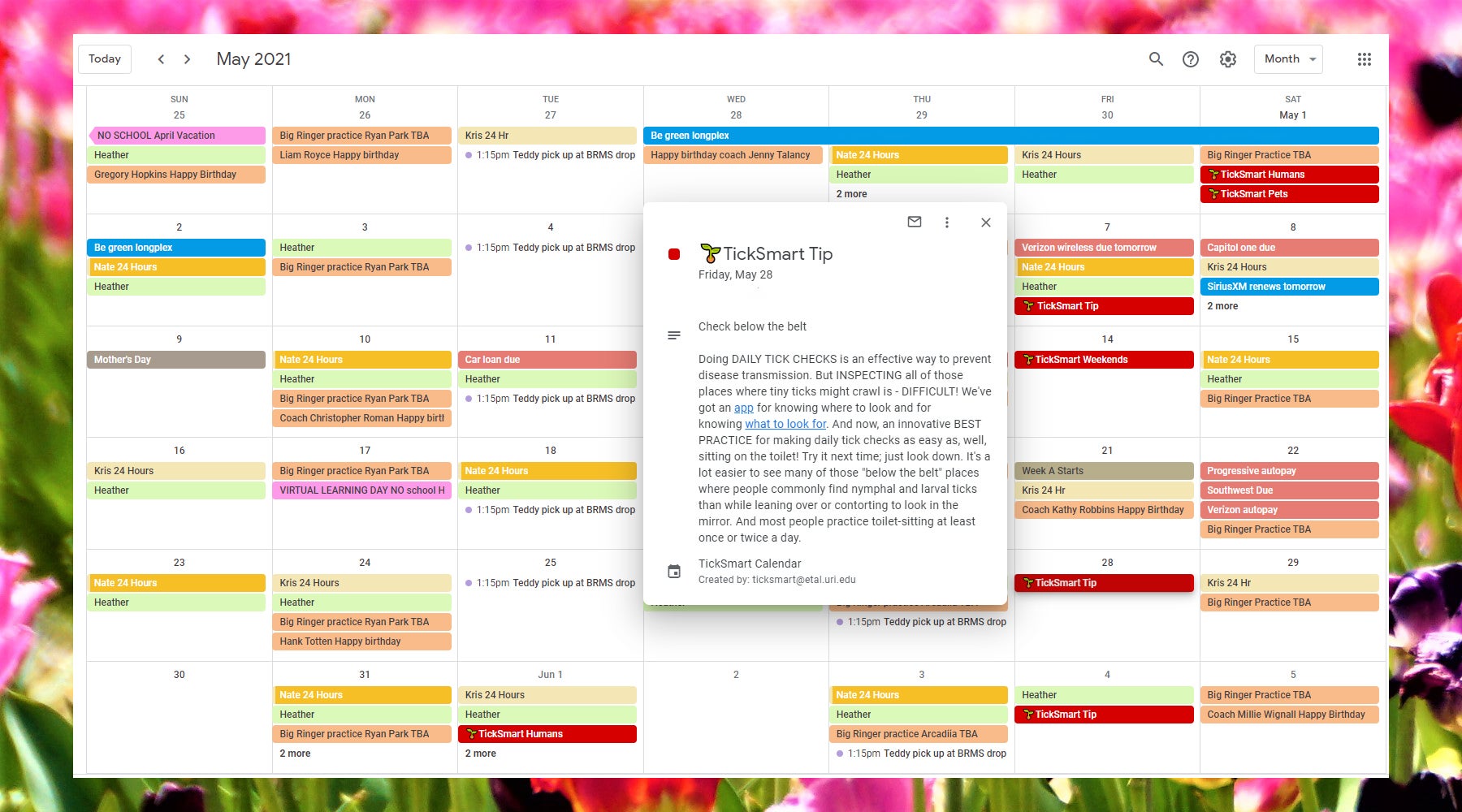
Everyday practices for TickSafe living

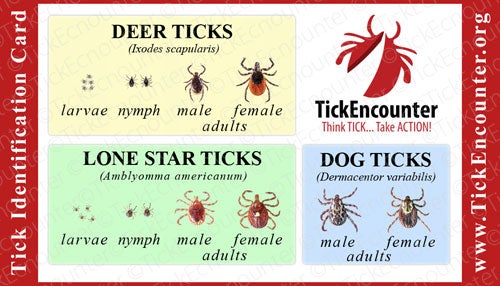
TickSmart™ focuses on providing people at risk for dangerous tick encounters with simple, effective strategies – everyday practices – for TickSafe living. Our goal is to make tick-bite protection easy so that you’ll actually “do it”.